Blog
A small message please try to spend quality time with your children, both DAD and moms especially dads. The more time you spend now when they are little, the more it will help in future. 1st three years a kid learns about his gender male or female, he learns how to self-soothe, self-control, what is real and what is not. It is a crisis how our children and teens are affected with the social media. Please leave your phones, tablets and TV when you are with your children. Please try to arrange some lectures on these issues. I want to be a part of this. Kindly let me know.
Thanks,
Dr. Muhammad Puri. Child and Adolescent Psychiatrist.
Now serving McKinney area ISD and communities.
Now serving McKinney area ISD and communities. Dr. Rehan Puri can serve as a liaison between school personnel, family, community and healthcare providers to advocate and facilitate the educational process. Dr. Puri can serve the safety of students and addresses the need for integrating health solutions into the education setting. Dr. Rehan Puri
- Advocates and provides health assessments and interventions for students and staff.
- Screens, evaluates and treat major psychiatric issues such as school avoidance, depression, anxiety and ADHD.
- Provides case management and education of students with chronic illness: Schizophrenia, Autism Spectrum Disorder, Intellectual Disability, ADD/ADHD.
- Administers medications to students when needed.
- Interprets the health status of pupils to parents and school personnel and coordinates information with schools and other health resources.
- Provides health education to students, staff, and parents.
- Provides leadership and is an integral part of the coordinated health teams
- Provides individual counseling with students and staff.
- Serves as a resource for physical and mental health promotion, accident and injury prevention and a safe school environment.
- Does school evaluation for students who need behavioral, 504 or I.E.P. treatment plan.
When to Contact a Mental Health Therapist or Child Psychiatrist in Allen
Mental health in Allen is important to us. As experts, we have seen many people go through difficult situations. When considering getting therapy in Allen for your child, you should be diligent. Here is a guide to help you make what could be the most important decision of your child's life:
When Is It Time to Seek a Psychiatrist in Allen?
Home Physical Abuse
It is unfortunate that a large part of the child population suffer from physical abuse at home. This can come in a variety of factors: parents or siblings hitting the child or shoving them. Physical abuse is always a call for therapy or mental help.
Home Sexual Abuse
While it is difficult to talk about, a child that has experienced sexual abuse may need psychiatric care right away. The long term damaging effects of abuse have been proven time and time again, and you can never start too late to help them.
School Physical Abuse
Sometimes it's hard to tell if your child has been abused at school. They often hide the marks and evidence because they don't want to face social consequences.
School Sexual Abuse
There are a number of situations where your child needs professional help from a psychiatrist in Allen, and sexual abuse at school is one of them. It happens more than you might think. Teachers, administrators, and other students can be the perpetrators of this, so ask your child if you think they may be a victim.
School Verbal Abuse (Bullying)
An often hidden form of abuse comes in verbal language by teachers speaking something out loud to the student during class where the rest of the students can hear. This can affect self esteem if not dealt with properly.
Familial Verbal Abuse
Inside your family, you may not realize, but kids have a unique way of adapting. If they don't feel they have power over the situation, they may not speak up if they feel you're abusing them emotionally or your spouse is. Sometimes, it can be visiting relatives that speak too harshly to the child.
Divorce
Children have a lot of stress when their parents separate. Often times, children report feeling like they are pawns used by either parent to play across the other. This creates inner tension and is likely to lead to problems down the road if they don't get the help they need.
Relationship Change
When your child starts having relationships with the same or opposite sex, they may feel very high one day and low the next. It's important to monitor their emotions. If you feel they are taking a break up hard, intervene by setting up a meeting with a mental health specialist.
Puberty
Puberty is a natural phase of life. However, the hormones created multiply and make teenagers feel many emotions in a short burst of time. It is not shameful to ask for help for your teenage child if they are in this stage of their development.
Loss of a Loved One
Few things are more psychologically taxing than losing someone you love. Often children report feeling confused, lost, abandoned, and even dreadful of the prospect of imminent death.
Body Issues
When a child is overweight, they may feel ashamed of this fact due to being teased at school or having someone point out the increased health risks associated with their condition.
General Self Esteem
Life isn't easy, even for children with wonderful parents. If you feel your child could use a boost of self esteem, there are healthy ways to engage with professionally without making them feel there is anything wrong with them.
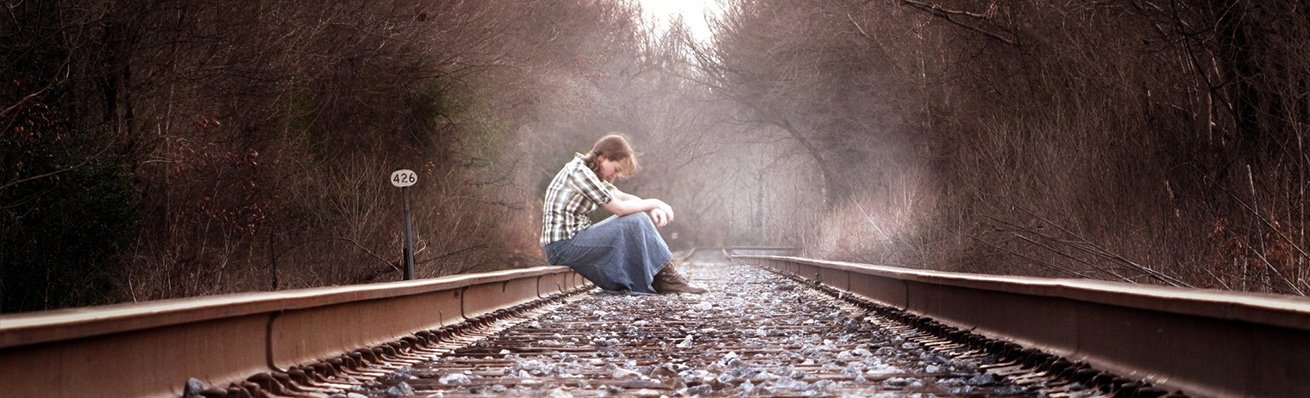
Signs of Self Harm
Wearing long clothing in hot months, sulking in their room, and generally avoiding showing skin is a sign that your child could be hiding cuts, bruises, or other self harm marks.
Claims of Intended Suicide
Often, claims of suicide are calls for help in disguise. Our professionals are ready to help your child if you even so much as suspect they could be in danger of taking their life.
Major Injury
After suffering a major injury, such as losing the use of a limb or tearing a ligament in high school sports, kids can get down pretty fast. It's not something they have to suffer through alone though.
Loss of Pet
Pets are often a member of the family, on the same level as any other loved on. Losing a pet suddenly can be disastrous for a young person. But it doesn't need to be.
Our Facilities for Mental Health in Allen
When it comes to caring for your child, we pride ourselves on providing the best possible facilities. We believe the surroundings of the child are important when being helped by a mental health professional.
We have state of the art facilities that are calming, clean, and professional. Our staff is licensed and experienced and we take the utmost attention to detail when helping your child, yourself, and the rest of your family through this difficult time.
Steps to Seeking Therapy in Allen
If you have realized that your child needs help, we are here for you. The next steps are to reach out to us and let us consult you on how we can help your child feel and live better. Schedule an appointment or walk in options both exist, depending on the circumstances.
When it comes to a child's psychology, there can be many things affecting them at any time. It's important to keep an eye on these things and be aware if they start acting strange. Use the guide above to get in touch with us for professional psychiatric help if you notice any strange signs from your child.
Prevalence, Assessment, and Management of Psychotropic Drug-Induced Movement Disorder in Pediatric Population
Muhammad Rehan Puri1, Shabber Agha Abbas2, Jennifer Zajac1, Salma Malik1, Charles Caley1
1Institue of Living, Hartford, CT.
ABSTRACT
OBJECTIVE: The study of psychotropic drug-induced extrapyramidal movement symptoms (EPS) adverse drug reactions (ADR) in the pediatric population is an area of growing concern given the increased frequency of prescription. This study was conducted to ascertain the prevalence and etiology of such cases and to evaluate identified risk factors in order to make appropriate management recommendations.
METHODS: A retrospective online PubMed search from the past 7-10 years was conducted looking for pediatric case studies reporting involuntary EPS following use of psychotropic medication. Identified cases were further evaluated on basis of standard demographic characteristics, acute versus chronic side effects, type of movement disorder, psychiatric diagnosis, type of psychotropic drug used, and ADR probability scaling using the Naranjo scale.
RESULTS: A total of 45 cases were identified with patients having a mean age of 13. The majority of patients were males (72%). Various offending psychotropic drugs were identified including second-generation anti-psychotics, antidepressants, and psychostimulants. Second-generation anti-psychotics were most commonly implicated (35 patients) and among them risperidone was most frequently used and quetiapine the least. Dystonia was reported in 44 patients and tardive dyskinesia in 1 patient. Mean of Naranjo scale scores was 5.57. Dystonia occurred early and late in roughly equal number of patients. In one case, tardive dyskinesia was reported after discontinuation of risperidone. In most cases the discontinuation of offending agent and use of an anticholinergic were sufficient to stop symptoms. In few cases dystonia reoccurred after restarting the medication.
CONCLUSIONS: Psychotropic medications do increase the vulnerability of the pediatric population to involuntary movement disorders. In particular, second-generation anti-psychotics, SSRIs, and stimulants should be prescribed with caution and should be closely monitored for symptom development. Development of treatment guidelines may help clinicians devise safer management strategies. Further research is needed to elaborate on the risks versus benefits prescribing these drugs for psychiatric disorders in children.
Abbreviations: SGA- Second Generation Antipsychotics, FGA- First Generation Antipsychotics, EPS- Extrapyramidal Side Effects, SSRI- Selective
INTRODUCTION
- Historically, anti-psychotic drugs have been used in children and adolescents infrequently due to safety concerns
- This rate of use has considerably increased largely due to increased availability of atypical anti-psychotics
- 65% increase from 2002 – 2009 (Health Services Research) (1)
- 38% increase according 2012 (JAMA) (2)
- Studies have also shown an increase in prescribing trends for attention deficit hyperactivity disorder (ADHD, conduct disorders, and affective disorders
OBJECTIVES
- The aim of this retrospective case review was:
- Describe the clinical presentation, pathogenesis and epidemiology of psychotropic induced movement disorders in childhood.
- Highlight our understanding of the underlying mechanisms of psychotropic movement disorders and to delineate avenues for future research in this area.
- Review some guidelines in pediatric setting for the use of psychotropics.
METHODS
- We identified published case reports within the past 10 years through ‘PubMed’ literature search
- Identified cases were reviewed by 3 psychiatrists
- Adverse Drug Reaction (ADR) Probability Scale was utilized for this purpose (developed by Naranjo)
- ADR Probability Scale consists of 10 items that are answered as either Yes, No, or “Do not know”
- Different point values (-1, 0, +1 or +2) are assigned to each item
- Total scores range from -4 to +13; with the reaction being considered definite if the score is 9 or higher, probable if 5 to 8, possible if 1 to 4, and doubtful if 0 or less
- Independent raters evaluated and scored each case independently
- Cases with individual scores that were not identical were then reconciled by the raters through discussion of the case in order to determine a single score
RESULTS
- Mean age of patients =13 years (13.12 ± 4.36)
- Median age = 14 yearsl range = (neonate to 18 years)
- 70% were male; 30% female; 1 case gender not delineated
- Total of 45 cases were identified in the literature
- 41 had generic dystonic reactions
- 4 were sub-classified as tardive, kinsergic, laryngeal, and writer’s dystonia
- In most cases, dystonia was reported following start of medication
- In few cases, dystonia was reported following treatment discontinuation
- In most cases, discontinuation of offending agent and use of anti-cholinergic medication were sufficient to stop symptoms
- In few cases, repeat dystonia occurred when medication was re-challenged
- Mean of Naranjo scores was 5.58 ± 2.00; Median was 5; Range was 1-11
- In majority of cases, 62.2% of patients (28/45) had Naranjo score > 5; 37.8% had score <4
- Description of cases (Table 1)
- Description of offending agents (Table 2)
Table 1 – Condition for Anti-Psychotic Medication Usage
Schizophrenia/psychosis: 16/45 (35.6%)
Bipolar/mania: 12/45 (26.7%)
ADHD: 8/45 (17.8%)
OCD: 3/45 (6.7%)
Autism: 3/45 (6.7%)
MDD/depression: 2/45 (4.4%)
Accidental: 2/45 (4.4%)
Other: 4/45 (8.9%)
Multiple: 7/45 (15.6%)
Table 2 – Movement Disorder-Inducing Agents
Atypical antipsychotics implicated in 35/45 (77.8%) cases
Aripiprazole: 8/35 cases [22.9%]
Olanzapine: 6/35 cases [17.1%]
Quetiapine: 4/3 cases [11.4%]
Risperidone: 11/35 cases [31.4%]
Ziprasidone: 6/35 cases [17.1%]
Antidepressants implicated in 8/45 cases (17.8%)
Stimulants implicated in 5/45 cases (11.1%)
DISCUSSION
- Mean Naranjo score of 5.58 provided a sufficient level of reassurance regarding the drug-related causality of the adverse event
- Dystonia was observed in both single-use and combination use
- Dystonia associated with SSRI use can be attributed to effects on caudate function and glutamate neurotransmission suggesting an increased risk of EPS in autistic disorder following SSRI exposure
- Atypical antipsychotics was responsible for the largest number of cases, amongst which Risperidone and Aripiprazole were responsible for more than half of all cases – reflecting increased prescribing trends rather than drug-specific adverse event predisposition
- Lower rates of drug-induced Parkinsonism was associated with Quetiapine suggesting potential use as drug of choice in adolescent population
- No typical anti-psychotic case identified likely due to drastically reduced prescribing trends over past 10 years
- Risk factors for developing ADRs including younger age, male population, familial disposition, polypharmacy, and high dosage
- Limitations of the study include lack of case controls, no measure of symptom severity, assumption of patient medication usage as indicated, controlling for psychotropic polypharmacy
- Pediatric patients being treated with psychotropic medication should receive complete periodic neurological examination to screen for potential adverse events
- Clinicians should learn to recognize and distinguish between development of movement disorders related to psychotropic drugs vs due to pathology as misdiagnosis can have serious treatment consequences
CONCLUSIONS
- Psychotropic drugs mainly antipsychotics increase the vulnerability of pediatric population to movement disorders
- Second-generation anti-psychotics are not free of EPS esp. Risperidone and Aripiprazole
- Other offenders are Fluoxetine, Citalopram, and stimulants
- These medications should be prescribed with caution in children and close monitoring is warranted by periodically performing movement disorder scales like AIMS,Barnes Akathisia Scale
- Development of a guideline to treat a dystonic reaction in child and adolescent populations and raising awareness regarding this adverse effect is crucial
- Further research is needed to evaluate the risk, benefits, and adverse effects of prescribing these drugs for psychiatric disorders in children
REFERENCES
- Matone M, Localio R, Huang YS, et al. The relationship between mental health diagnosis and treatment with second-generation antipsychotics over time: a national study of U.S. Medicaid-enrolled children. Health Serv Res. 2012;47(5):1836-1860.
- Kreider AR, Matone M, Bellonci C, et al. Growth in the concurrent use of antipsychotics with other psychotropic medications in Medicaid-enrolled children. J Am Acad Child Adolesc Psychiatry. 2014;53(9):960-970.